The history of contagious diseases and their epidemic outbreaks is a field of scientific research that falls not only within the scope of life sciences (medicine, biology) but also social sciences. Indeed, historiography allows us to discern the intertwinement of epidemics with the evolution of human societies, by analyzing how these impacted each time on various activities and thus required the reconfiguration of different social resources (spatial, material, cognitive, human). Far from ascribing to epidemics an overarching causative power, one cannot fail to note how these turned out to be decisive in various historical conjunctures by speeding up or slowing down wars, economic competitions, migrations etc. In fact, experts in global history suggest epidemics and their different temporalities could stand as an additional interpretative tool in regards to long term shifts of global power, e.g. from Asia to Europe since the 13th century, as well as the colonial rule of western powers on a global scale (Grmek 1963, Lippman Abu Lughod 1994, Diamond 1997).
On a same note, the long modernizing process that began in Western Europe rendered public health management an indispensable condition for the constitution of national populations, which overall had to be healthy, literate, registered in national statistics, integrated in the labor market and adapted to civic duties (in peacetime and war alike). The social management of public health in the era of modernity is perhaps best exemplified with the emergence of the scientific fields of epidemiology and medical geography —with their related Societies, scientific publications etc.—, as well as various other new technologies relative to public hygiene and the optimization of yield on public investments (urbanism, engineering, sociology, education etc.). Moreover, the first waves of European colonization gave a significant momentum to the study of epidemics; writing on the close relationship between epidemiology, medical geography, and European expansion, French-Croat historian Mirko D. Grmek noted that already since the 17th century “the age of great geographical discoveries awakes interest for new skies and ‘exotic pathology’. Tropical medicine, the new branch of Medicine, is born” (Grmek 1963). The underlying rationale of such domestic processes will be accentuated by the worsening of international competition in the second half of the 19th century, the age of grave economic crises and relentless colonial expansion. In fact, the central importance of large military units and their constant relocations in new environmental conditions often entailed the outbreak of epidemics among native populations or newcomer troops; this continuous spatial and human reconfiguration on a global scale led to the establishment of a scientific tradition of epidemiology and medical geography within the military and colonial domain.

The First World War was the outcome of this long process of technological, political and military globalization. On an epidemiological level, the study and prevention of epidemics among military and civilian populations took on an unprecedented scale, given the technological advances of the time, the military stakes of the Great War, the scope of epidemics caused by the relocation of millions of soldiers in new environments and unsanitary conditions (see malaria in the case of stagnant waters), as well as the outbreak of the so-called “Spanish influenza”. The latter broke out towards the end of the War and peaked in 1918 (Lina 2008); this pandemic is also credited with the premature end of the War, given it was particularly devastating among adults aged 20 to 40 years old, with a worldwide fatality toll up to 50 millions. Its geographical origins are still contested —either Eastern Asia or North America (Lina 2008). In fact, the new emerging means of communication and transport of the time rendered this pandemic even more independent in regards to traditional spatial and temporal limits. Hence, it illustrated in a rather morbid way the new globalized reality which national States and their respective scientific apparatuses had to deal with. The latter were called to effectively overcome their partial national interests and gradually work towards the consolidation of an actual international community for the study and the prevention of epidemics (Grmek 1963). Of course, this international community would come to materialize only after Second World War and the defeat of the Nazi project and its own “version” of medical geography (Geomedizin).
The deadly but also extremely cosmopolite experience of the First World War functioned as a costly precedent, that enabled a large number of scientists —civilians and military— to conduct innovative researches with significant results. In these particular conditions, Greece —and more specifically the Greek region of Macedonia, where the famous Armée d’Orient was stationed and fought under French command— proved to be an epicenter for global research and anti-epidemic struggle, involving large numbers of foreign and Greek specialists, and thus speeding up the modernization of sanitation policies in Greece. This modernization would become even more urgent with the territorial expansion of Greece throughout this period, as well as the arrival of hundreds of thousands of Greek refugees following the Minor Asia Catastrophe of 1922.
“Epidemy” is a Greek word
Located in the geographical margins of Western Europe, the Modern Greek State had been a constitutive part of European modernity since its founding in 1830 and held close political, scientific, and economic ties with major European powers of the time (France, United Kingdom, Germany, Italy). Far from being a simple relic of the past in the western imaginary, Greece stood as a modernizing force in South-East Europe. Furthermore, climate conditions in the Balkans and recurring contagious diseases such as malaria had rendered early on the prevention of epidemics a pressing issue, in parallel to international developments.
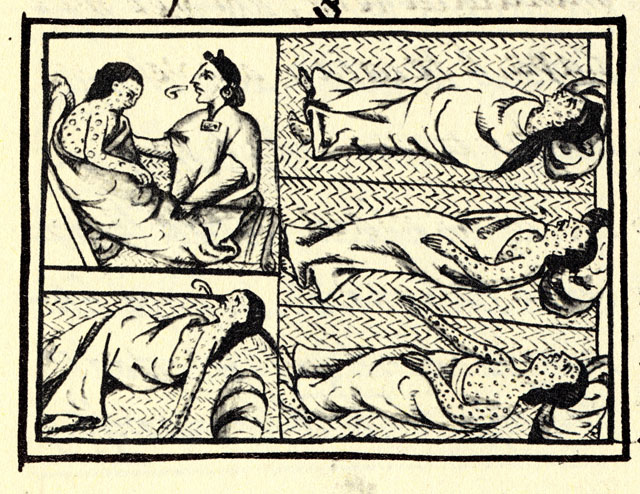
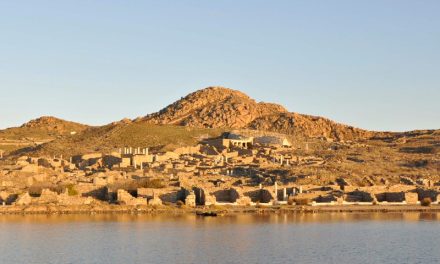
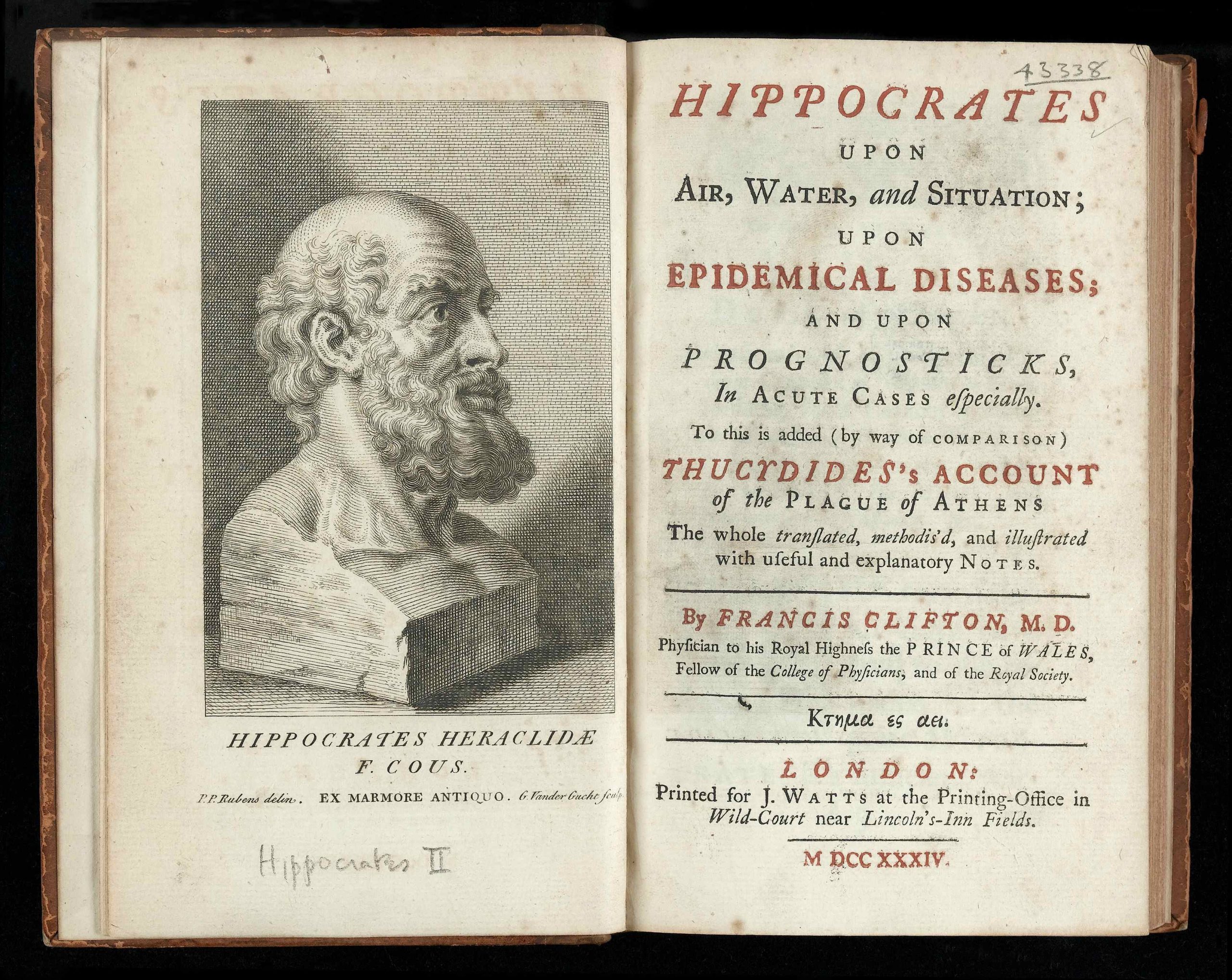
The discipline of medicine itself can be traced back to ancient Greece and more particularly to Hippocrates of Cos (ca 460-377 BCE), who lived during the golden age of Pericles; Hippocrates delivered indeed detailed descriptions of infectious diseases —including a potential case of an influenza epidemic in Thrace around 410 BCE in his Sixth book of Epidemics (Lina 2008, Pappas et al 2008). However, it is malaria that seems to have had a larger historical impact. According to noted British classicist W.H.S. Jones’ hypothesis, malaria may have reached such an extended epidemic scale during classical times that it might have actually contributed to the loss of power of Greek cities on a regional level; the origins of malaria epidemics in ancient Greece have indeed been an issue of debate among historians for a long time (see Grmek 1983). To be noted that Jones had articulated his arguments while working in Greece along British epidemiologist and Nobel-prize winner Ronald Ross, himself invited in 1906 to work on the grounds of Lake Copaïs by the private company that was in charge of the famous drainage project (Grmek 1963, 1983).
Indeed, malaria had had an endemic presence in various regions of Greece due to specific ecological conditions and remained a defining characteristic of the social history of Greece throughout centuries. As noted by one of the pioneers of Greek medical history, Aristotelis Stavropoulos, malaria was the prevalent disease in the Hellenic space, with a high-rate of mortality and recurrent epidemic outbreaks (Stavropoulos 1982). Historical research allows us even to revisit certain well-known historical epidemics under the light of malaria (see Gounaris 2008 on the epidemic of 1783 in Salonica). In general epidemiological terms, one can conclude, as noted by Stavropoulos —an advocate of the theory of continuity of Greek medicine throughout history—, that Greek communities of the Ottoman Empire seem to have been well prepared against plague or smallpox epidemics because of their intellectual contacts with Western Europe, as well as their own communal traditions (Stavropoulos 1982). Nonetheless, in the long term, malaria constituted a real challenge (endemic with epidemic potential and outbreaks), which Greece would need to confront, once liberated.
The founding father of medical geography, French military medical doctor Jean Marc Christian Boudin had himself witnessed the devastation caused by malaria upon French troops during their expédition du Morée in aid to the Greek Revolutionaries against the Ottomans in the Peloponnese in 1828, a couple of years before the founding of the Modern Greek State (Boudin 1842, Grmek 1963); as he wrote, “after having observed the malarious fevers in various places in France, in Germany and Spain, I became witness during the French expedition in the Morée in 1828 of this dismal tragedy that took place in the swamps of Navarin, where I saw our army decimated in the most cruel manner without even having fought, due to an unforgivable oversight of all hygiene rules”(Boudin 1842).

Nonetheless, despite the fact that malaria would continue to prevail —for example, the city of Athens would undergo 14 large scale malaria epidemics in the period from 1860 to 1905— there was no real anti-malaria initiative in Greece during the second half of 19th century, apart from some seminars for limited audiences (Mandyla et al 2011); the country seemed to be under siege by malaria throughout this period, a problem that became all the more aggravated by its impact on the health condition of the Greek army, much needed at a time of territorial aspirations. This problematic was first of all formulated by members of civil society and most notably engaged scientists, such as Professors Savvas and Kardamatis, who took the initiative of founding in 1905 the Greek Anti-Malaria League, closely linked with the Italian one. The Greek League started its action right away and was immediately endorsed by King George I. However, its activities relied solely on its own initiatives and voluntarism, without any actual coordination on behalf of the public administration. In any case, it seems that in parallel to the first practical contributions of the League (sanitation campaigns, legislation of state monopoly on quinine, drainages), its social education and mobilisation campaign was equally significant, given that it contributed to raising awareness among a large part of the Greek population in regards to the prevention of malaria epidemics and, we could add, epidemics in general (Mandyla et al 2011). The constitution of epidemics into a social problematic with a given mobilizing power would prove to be important in the future (also see the works of Katerina Gardikas 2008, 2018 and the thesis of Maria Vassiliou 2005)
However, right at the turn of the 20th century, the management of malaria epidemics in Greece would also prove to be a much more complex issue than a simple debate of national hygiene: despite its nominal neutral status, Greece, and more specifically the newly liberated Greek region of Macedonia and the cosmopolite city of Thessaloniki, would be abruptly introduced in the First World War in 1915 with the landing of Entente forces and the formation of the famous Armée d’Orient on the Macedonian front under French command. The political and scientific stakes of the anti-epidemic struggle on the Macedonian plains suddenly exceeded local or national confines, and became part of a wider web of geopolitics, diplomacy, and military science.
Tropical Salonica
The population residing in Salonica and its surroundings reached 600.000 from just 120.000 (Mikanowski 2012). Malaria, or “disease number 11” as it was called by the French army at the time, quickly proved to be a fearsome enemy during the summer of 1916 (Bernède 1998). Even though the mortality rate was relatively limited (Mikanowski 2012), the impact on the combat readiness of Allied troops was incommensurable, since thousands were hospitalized. Commander of Allied Troops, French General Maurice Sarrail had to deal with this problem; since the very start of the installation of the troops an immense logistics operation was put in place in order to provide the Entente soldiers all the needed infrastructure without them having to requisition any installation from the locals and thus risk turning into occupation forces. This contributed to the completion of important public works in Salonica and the surrounding area (roads, railroads, clean drinkable water network, drainages). This operation even meant French forces started cultivating their own vegetables in order to fulfill their nutritional needs in times of epidemics, a practice that nonetheless drew the sarcastic comment of then French Prime Minister Georges Clémenceau who called them “gardeners of Salonica” (Bernède 1998).
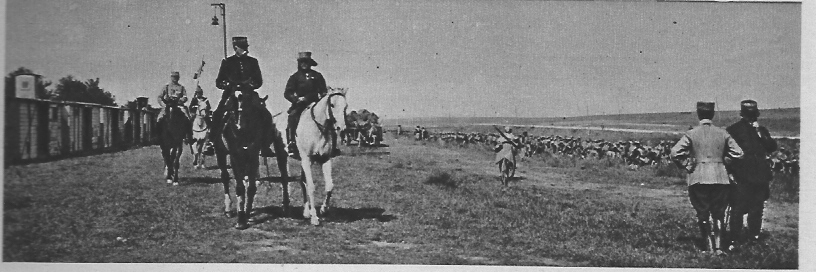 Zeitenlik base; French troops parade in front of generals Bailloud et Sarrail. Le Miroir n.104, page 5, 21 November 1915 (Source: Wikimedia Commons)
Zeitenlik base; French troops parade in front of generals Bailloud et Sarrail. Le Miroir n.104, page 5, 21 November 1915 (Source: Wikimedia Commons)Besides this great effort of logistical support, the threat of malaria and its first epidemic outbreak alarmed Entente troops, who called their best specialists in tropical medicine (from Ronald Ross to the Sergent brothers of the Pasteurs Institutes in North Africa). In fact, as playfully pointed out by Jakob Mikanowski, the Macedonian front “was in Europe, but was not European”, due to fact that a large part of western troops consisted of soldiers from colonies (Western Africa, Madagascar), while for French or British officers the climate and the heat of the country resembled those of their previous colonial experiences (Mikanowski 2012). To add to this, Salonica was a multi-ethnic city at the time, a further element of exoticism in the eyes of newcomers (White 1920). However, once on site, western medical personnel collaborated with their local and colonial counterparts; according to Jacob Mikanowski, Salonica constituted de facto a real human laboratory for epidemiologists of all sorts who combined diverse approaches in their efforts to counter malaria (either based on quinine treatment or vector-control approaches). The work of these specialists did not only concern military but, of course, also civilian populations; the Entente forces also took part in the administration of the city. On a strictly medical level, the Medical Society of Salonica was the main forum for discussion and knowledge sharing among Greek and foreign specialists, military and civilians alike. Jacob Mikanowski points out that the vast medical and epidemiological community that was formed in Salonica exceeded the scope of anti-malaria and the confines of tropical medicine, reaching thus a remarkable level of scientific innovation with universal implications, as exemplified with the case of Ludwik Hirszfeld (see Mikanowski 2012).
 Justin Godart having a discussion with Princess Narychkine, founder of the hospital on the Macedonian Front, 1917 (Source: Wikimedia Commons/ Service Photographique de l’Armée d’Orient)
Justin Godart having a discussion with Princess Narychkine, founder of the hospital on the Macedonian Front, 1917 (Source: Wikimedia Commons/ Service Photographique de l’Armée d’Orient) The experience of the First World War and the presence of Allied forces left their imprint in Northern Greece; following the Great Fire of Salonica in 1917, the new city plan was trusted by Greek statesman Elefthérios Venizelos to French urbanist Ernest Hébrard. The new plan, rectangular and in compliance with the modern precepts of public hygiene marked a new turn for the city (Lagopoulos 2005). Moreover, the anti-epidemic struggle in Northern Greece in the aftermath of the war was influenced by the wartime experience of international cooperation, as demonstrated for example by the collaboration of Greek authorities with the mission of the American Red Cross in Macedonia (White 1920). To add to this, the Great Catastrophe of 1922 and the advent of hundreds of thousands of refugees entailed the implication of the international community for their support. In brief, these radical social changes and required sanitation reforms necessitated the mobilisation of Greek authorities and the transition to a systematic anti-epidemic State policy since the late 1920s, especially in the case of malaria, initially in collaboration with the Greek Anti-malaria League but also later with institutions such as the Rockefeller Foundation or the United Nations (UNRRA) (Gardikas 2008, 2018, Mandyla et al 2011).
This historical turn allowed Greek society and State to constitute the fight against malaria a “national cause” while at the same time taking part in the international anti-epidemic scientific community, under consolidation right in the aftermath of the Great War and the so-called “Spanish influenza” pandemic (Tsoucalas et al 2015, Tsoucalas et al 2016, Lina 2008, Grmek 1963). This shared awareness on epidemics would serve as a precious precedent in Greece for generations to come.
Originally written for grecehebdo.gr in French & adapted into English by Dimitris Gkintidis.
D.G.
TAGS: ENVIRONMENT | FOREIGN AFFAIRS | HEALTH | HISTORY | INNOVATION | SCIENCE & TECHNOLOGY